The legislation established 15 required components of a comprehensive EMS system—including manpower, training, communications, transportation, trauma care facilities, public safety agencies, and consumer participation. It helped transform fragmented local responses into coordinated systems with regional medical control.
The Act authorized up to $185 million for planning, creation, and expansion of EMS systems. Unlike the Highway Safety Act of 1966, which made grants available only to states, the 1973 Act specified that states, local governments, public entities, and nonprofit private entities were all eligible for direct funding. First-year grants required 50-50 matching; subsequent grants required 75% nonfederal contribution. Congress defined an EMS system in terms of fifteen specific functions and treated all fifteen as mandatory.
President Nixon initially vetoed the legislation, arguing for a continued limited federal demonstration role. The Senate overrode, but the House sustained the veto. Congress reintroduced and Nixon signed P.L. 93-154 on November 16, 1973. The Act passed less than one year into the five-site demonstration phase launched by Nixon's own 1972 Health Message — before demonstration results were available.
View source (EMS History PDF)
Source: Gibson, Geoffrey. "Emergency Medical Services." Proceedings of the Academy of Political Science, 1977 (PDF)
Source: Hanlon, John J. "Emergency Medical Services: New Program for Old Problem." Health Services Reports, March 1973 (PDF)





 Image: Dr. Eugene Nagel and early Miami paramedic team – Source: EMS History
Image: Dr. Eugene Nagel and early Miami paramedic team – Source: EMS History




 Image: President Richard Nixon – Source: Constant Contact Archive
Image: President Richard Nixon – Source: Constant Contact Archive



:max_bytes(150000):strip_icc()/lyndon-b--johnson-at-press-conference-515418542-9be0f70bbcdb4fc389de1d0941ec77e7.jpg) In April 1972, former U.S. President Lyndon B. Johnson suffered a heart attack at his ranch near Charlottesville, Virginia. Volunteer EMTs from the Charlottesville–Albemarle Rescue Squad, including Nathaniel P. Rogers, responded to the call and utilized their new LifePak 33 defibrillator to obtain a 12-lead electrocardiogram (ECG) in the field. He was then treated under the direction of Dr. Richard S. Crampton at the University of Virginia.
In April 1972, former U.S. President Lyndon B. Johnson suffered a heart attack at his ranch near Charlottesville, Virginia. Volunteer EMTs from the Charlottesville–Albemarle Rescue Squad, including Nathaniel P. Rogers, responded to the call and utilized their new LifePak 33 defibrillator to obtain a 12-lead electrocardiogram (ECG) in the field. He was then treated under the direction of Dr. Richard S. Crampton at the University of Virginia.
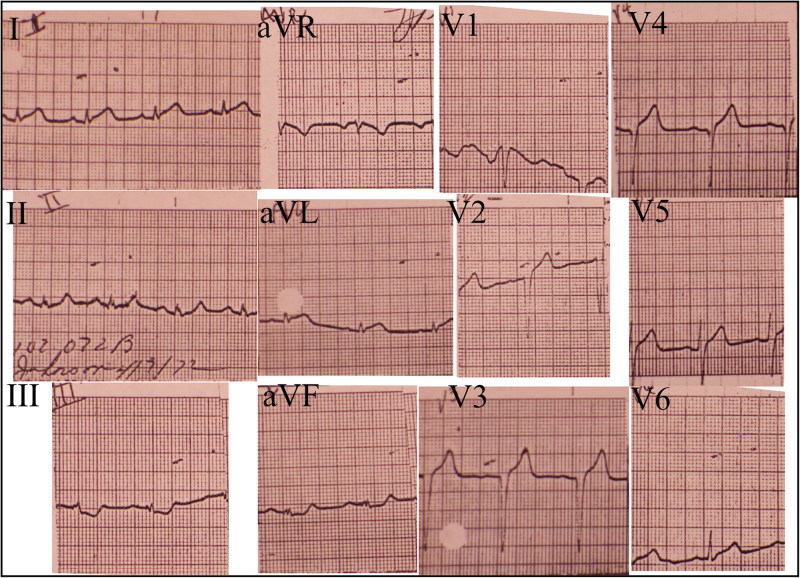

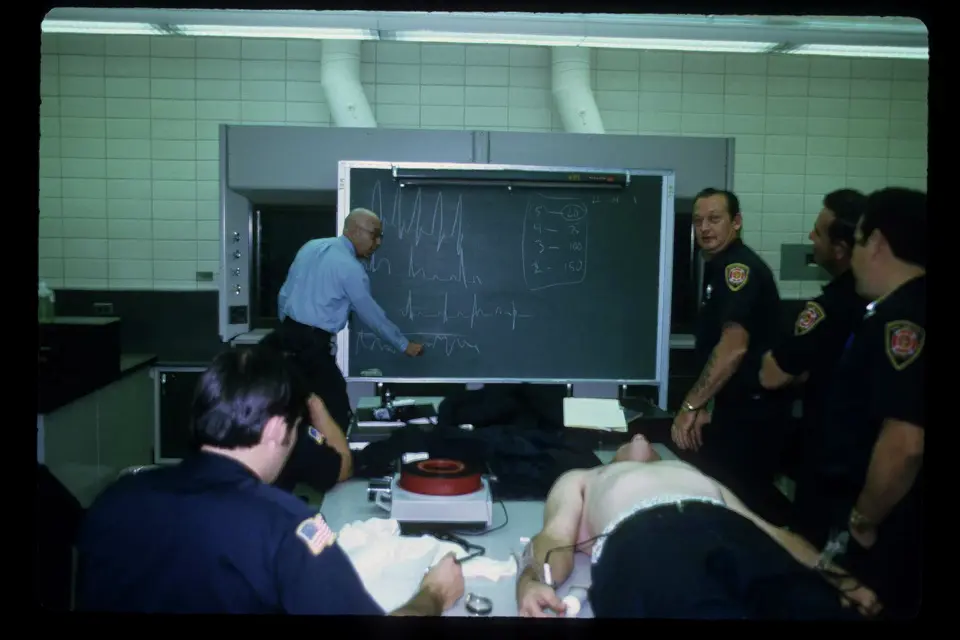








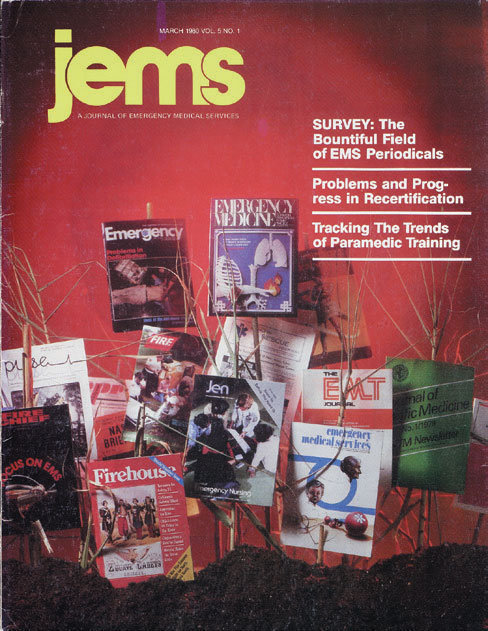 Image: The first cover of JEMS – Source: National EMS Museum
Image: The first cover of JEMS – Source: National EMS Museum
